The Meaningless Diagnosis
As healthcare providers, we are tasked with figuring out a diagnosis and what the best approach to treat it is. As our understanding of pain science and biomechanics improves, our diagnoses should reflect these changes leading to improved outcomes.Unfortunately, there are many diagnoses that are given to explain why someone is experiencing pain which do not reflect our current understanding of the body. Below are some of the diagnoses that do not adequately explain why someone is experiencing pain and may actually make someone worse.
Anterior Pelvic Tilt
 Anterior pelvic tilt is a common reason given for the development of lower back pain. Anterior pelvic tilt, also called lower cross syndrome, is a syndrome that describes tightness in the hip flexor and lumbar paraspinal muscles and weakness in the abdominal and gluteal muscles. The theory is this anterior pelvic tilt causes excessive lumbar extension and increased compression of the joints leading to pain.The problem with attributing an anterior pelvic tilt as the cause of lower back pain is that it may only be associated with pain, but not actually cause pain. For an anterior pelvic tilt to be clinically relevant, it would need to be present only during a painful episode and absent when someone is pain-free. However, an anterior pelvic tilt is commonly seen in asymptomatic individuals making it difficult to prove that the presence of an anterior pelvic tilt caused the low back pain.There is also a large range of lumbar lordosis found in the general population. A hyperlordosis in one person may actually be a normal lordosis in another person, with no relationship to the development of low back pain. The presence of pain has also been shown to alter movement, which means that when someone is experiencing low back pain their anterior pelvic tilt may increase or decrease to help relieve the painful episode.
Anterior pelvic tilt is a common reason given for the development of lower back pain. Anterior pelvic tilt, also called lower cross syndrome, is a syndrome that describes tightness in the hip flexor and lumbar paraspinal muscles and weakness in the abdominal and gluteal muscles. The theory is this anterior pelvic tilt causes excessive lumbar extension and increased compression of the joints leading to pain.The problem with attributing an anterior pelvic tilt as the cause of lower back pain is that it may only be associated with pain, but not actually cause pain. For an anterior pelvic tilt to be clinically relevant, it would need to be present only during a painful episode and absent when someone is pain-free. However, an anterior pelvic tilt is commonly seen in asymptomatic individuals making it difficult to prove that the presence of an anterior pelvic tilt caused the low back pain.There is also a large range of lumbar lordosis found in the general population. A hyperlordosis in one person may actually be a normal lordosis in another person, with no relationship to the development of low back pain. The presence of pain has also been shown to alter movement, which means that when someone is experiencing low back pain their anterior pelvic tilt may increase or decrease to help relieve the painful episode.
Forward Head Posture
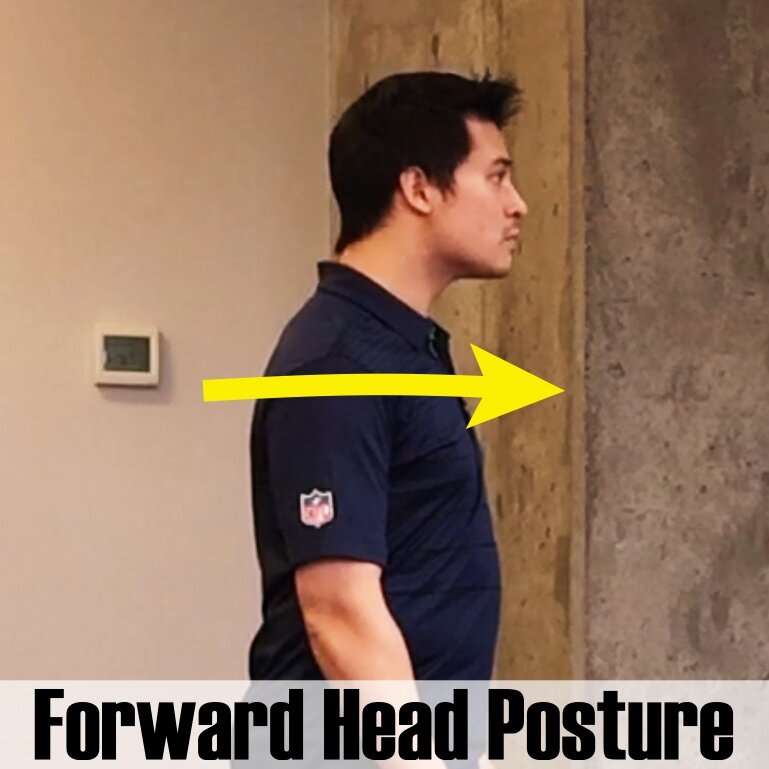 Forward head posture, also referred to as upper cross syndrome, is a condition similar to anterior pelvic tilt but is used to explain cervical and thoracic pain. For this condition, the combination of tight pectorals and sub-occipital muscles along with weak deep neck flexors and rhomboid muscles leads to compression of the facet joints in the cervical spine and pain.The development of forward head posture occurs over a prolonged period of time, therefore, the body has had adequate amount of time to adapt to these stresses and is able to tolerate these loads. So why would pain all of a sudden start because of a forward head posture? Did the forward head posture suddenly change when the pain began or did it progress so far that the body isn’t able to tolerate the load? In most scenarios the forward head posture has not changed, and similar to anterior pelvic tilt, the forward head posture may have been present before pain and is just a coincidental finding.
Forward head posture, also referred to as upper cross syndrome, is a condition similar to anterior pelvic tilt but is used to explain cervical and thoracic pain. For this condition, the combination of tight pectorals and sub-occipital muscles along with weak deep neck flexors and rhomboid muscles leads to compression of the facet joints in the cervical spine and pain.The development of forward head posture occurs over a prolonged period of time, therefore, the body has had adequate amount of time to adapt to these stresses and is able to tolerate these loads. So why would pain all of a sudden start because of a forward head posture? Did the forward head posture suddenly change when the pain began or did it progress so far that the body isn’t able to tolerate the load? In most scenarios the forward head posture has not changed, and similar to anterior pelvic tilt, the forward head posture may have been present before pain and is just a coincidental finding.
Overpronation
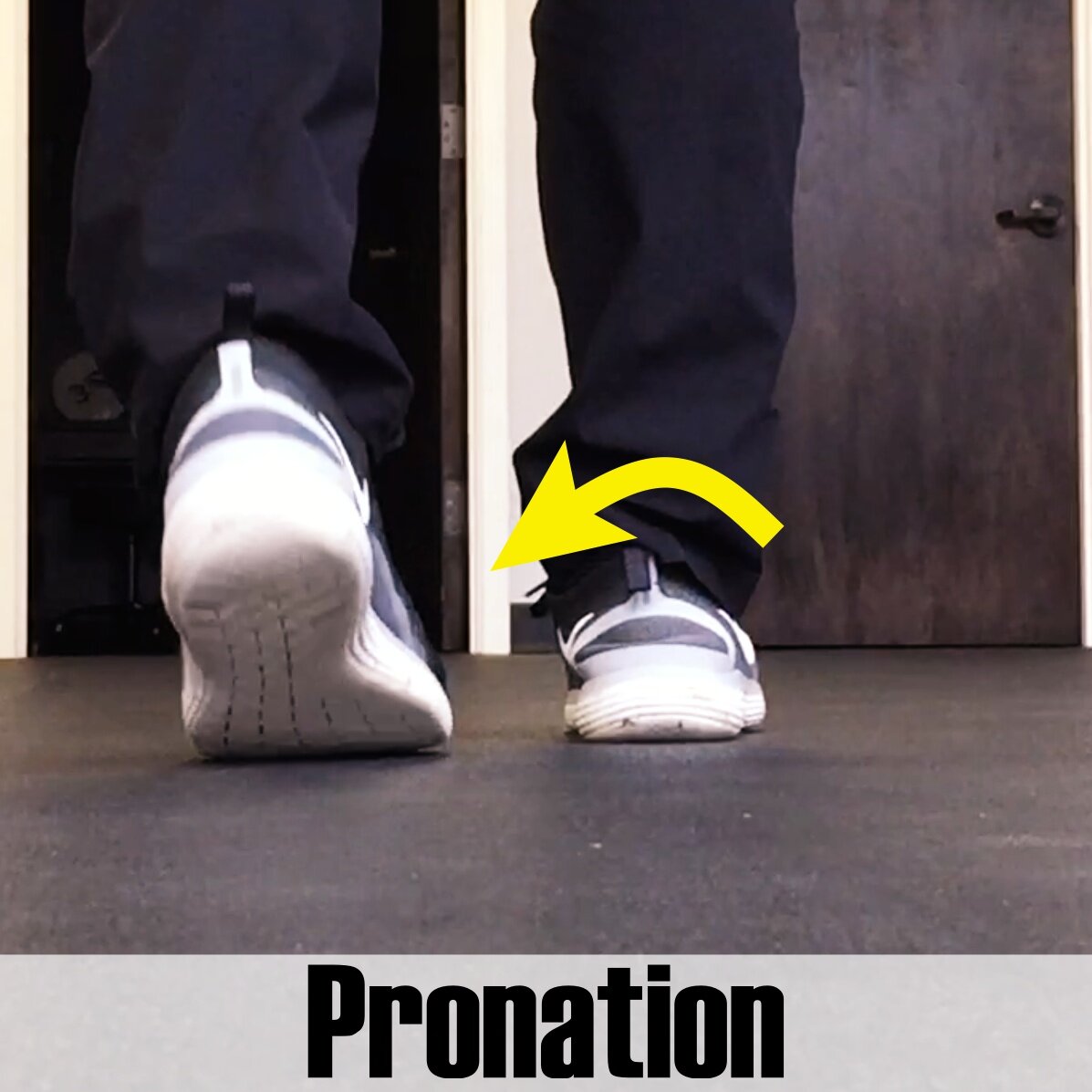 Pronation and foot pain, such as plantar fasciitis, is another example of a movement that is attributed to pain. The term pronation describes the combination of ankle dorsiflexion, abduction, and eversion. The truth is, 100% of those who have pain in their foot will pronate to some degree. Pronation is part of the normal gait cycle as the foot makes contact with the ground.Either the amount of pronation, termed over-pronation, or the rate of pronation is the explanation of why pronation would cause foot pain. Again, the question is either at what amount of pronation or at what rate of pronation does this movement become pathological? Since there is so much variety in gait patterns between individuals, it is difficult to say when something is pathologic or when something is normal. Even if pronation were the cause of pain, these movements occur so quickly it would be difficult for a clinician to measure either how much pronation or how quick pronation occurs making it difficult to determine if the movement is normal or pathological in the clinical setting.
Pronation and foot pain, such as plantar fasciitis, is another example of a movement that is attributed to pain. The term pronation describes the combination of ankle dorsiflexion, abduction, and eversion. The truth is, 100% of those who have pain in their foot will pronate to some degree. Pronation is part of the normal gait cycle as the foot makes contact with the ground.Either the amount of pronation, termed over-pronation, or the rate of pronation is the explanation of why pronation would cause foot pain. Again, the question is either at what amount of pronation or at what rate of pronation does this movement become pathological? Since there is so much variety in gait patterns between individuals, it is difficult to say when something is pathologic or when something is normal. Even if pronation were the cause of pain, these movements occur so quickly it would be difficult for a clinician to measure either how much pronation or how quick pronation occurs making it difficult to determine if the movement is normal or pathological in the clinical setting.
Conclusion
These diagnoses are commonly given to explain why someone is experiencing pain, however, they are not congruent with our current understanding of the body. Anterior pelvic tilt, forward head posture, and pronation are all normal movements and do not need to be medicalized. As healthcare providers, when we tell someone that an anterior pelvic tilt or overpronation are the cause of pain, patients naturally try to avoid these positions and movements. This can cause iatrogenic fear avoidance behaviors, possibly leading to worse treatment outcomes.Since these diagnoses provide little insight into the cause of pain syndromes and may actually act as an unnecessary nocebo, maybe it is time to consider changing our diagnosis to better reflect our understanding of the human body.